Let's see the glimpse below,
- Introduction
- The Healthcare Operations Landscape
- Understanding No-Code Technology
- Real-World Impact: No-Code in Healthcare Operations
- Platform Spotlight: Yoroflow in Healthcare Automation
- Overcoming the Barriers to Adoption
- Action Guide: Getting Started with No-Code
- The Time Is Now: Transforming Healthcare Operations with No-Code
Introduction
In a world where every second can make a difference in patient outcomes, the healthcare industry can no longer afford slow, rigid, and outdated operational systems. Hospitals, clinics, and healthcare providers face mounting pressure-not just from patient expectations, but from regulatory bodies, labor shortages, and cost constraints.
Nearly 75% of hospitals in the U.S. are experiencing critical staffing shortages, particularly among nurses and administrative personnel, according to the American Hospital Association's 2023 report. At the same time, operational inefficiencies are costing global healthcare systems up to $12 billion annually, as noted in a 2022 McKinsey & Company study. These inefficiencies are not merely financial-they affect the speed and quality of patient care, often leading to treatment delays and burnout among healthcare workers.
Traditional approaches to digital transformation have only compounded these challenges. The 2023 HIMSS Analytics Healthcare IT Implementation Survey found that most healthcare IT projects face delays of 6 to 12 months, with budgets exceeding estimates by over 30%. The root cause? A heavy reliance on traditional, code-based software development methods that require specialized technical teams and long implementation cycles.
But there's a quiet revolution underway: no-code technology-the ability to build applications and workflows without writing a single line of code. This new paradigm shifts the power of innovation from developers to domain experts, enabling healthcare teams to respond faster, customize solutions on the fly, and streamline operations with minimal IT dependency.
The Healthcare Operations Landscape
In the intricate world of healthcare, clinical excellence is only one side of the equation. Equally critical-yet often overlooked-are the behind-the-scenes operational workflows that support care delivery. These workflows touch every facet of the patient's journey, from scheduling and billing to records management and compliance.
When these systems operate efficiently, healthcare professionals can devote more time to what matters most: patient care. But when they falter, the consequences ripple across the entire organization, leading to delayed treatments, overburdened staff, rising operational costs, and even compromised patient outcomes.
Typical Healthcare Workflows
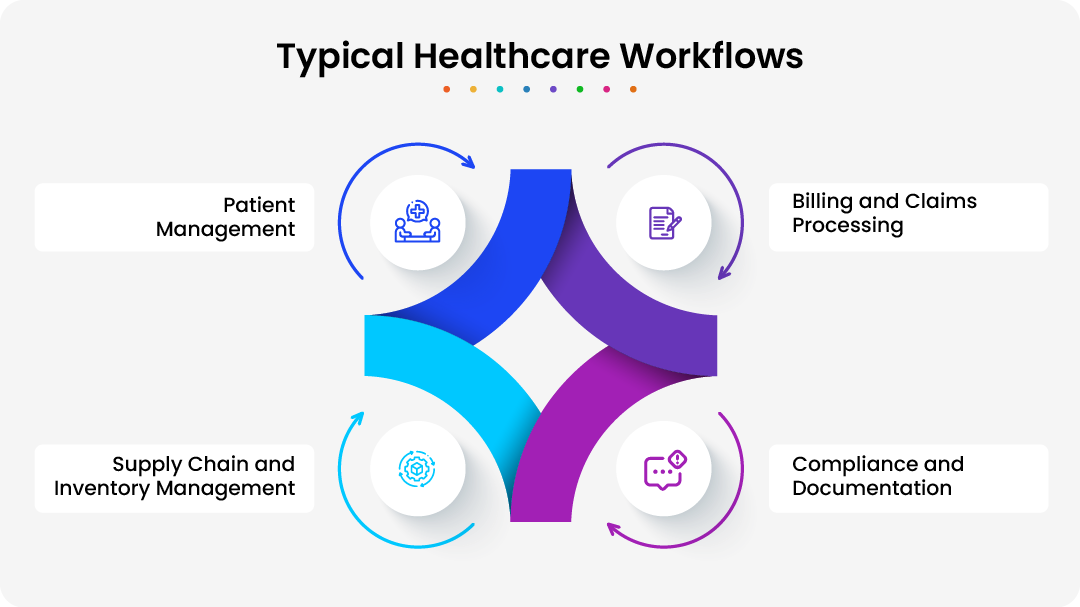
Healthcare organizations rely on a wide range of interconnected workflows to function smoothly. Some of the most common include:
Patient Management
This includes appointment scheduling, check-in processes, patient triage, care coordination, referrals, discharge planning, and follow-up care. These workflows must be both patient-centric and flexible to handle varying needs.
Billing and Claims Processing
Revenue cycle operations involve insurance verification, coding, claim submissions, rejections, appeals, and patient billing. Accuracy and timeliness are crucial to maintaining financial stability.
Compliance and Documentation
Healthcare providers must comply with numerous regulations such as HIPAA, CMS rules, and local laws. This requires diligent tracking of patient consent, staff certifications, policy updates, audit trials, and incident reports.
Supply Chain and Inventory Management
Hospitals and clinics must maintain essential medical supplies, medications, and equipment. Procurement, inventory alerts, expiration tracking, and vendor coordination are all vital operational components.
Each of these workflows typically involves multiple stakeholders-from frontline staff to administrators and IT teams-working across siloed systems with varying degrees of visibility.
Common Pain Points in Healthcare Operations
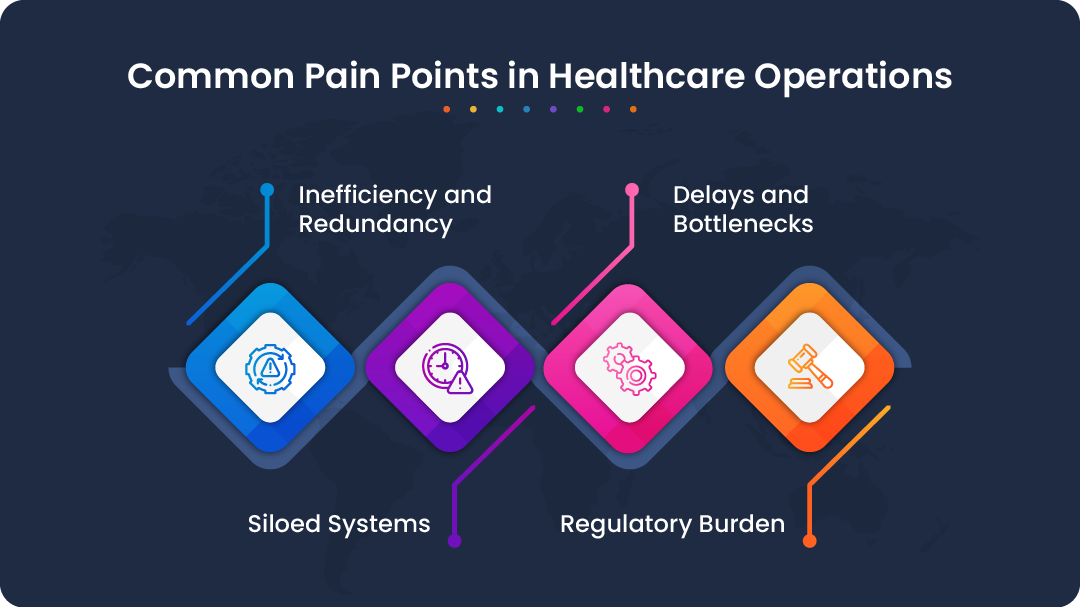
Despite advances in clinical care and technology, healthcare operations are still plagued by systemic inefficiencies. The most persistent issues include:
Inefficiency and Redundancy
Many organizations continue to rely on paper-based forms, email threads, spreadsheets, and disconnected tools. Repetitive data entry, manual task routing, and fragmented communications waste valuable time and introduce errors.
Delays and Bottlenecks
From delayed approvals to missed follow-ups, manual workflows frequently result in long turnaround times. These delays disrupt patient flow, impact resource availability, and strain staff capacity.
Siloed Systems
Most healthcare systems use a patchwork of electronic health records (EHRs), scheduling tools, HR systems, and third-party software that do not communicate with each other effectively. This fragmentation creates data blind spots, slows decision-making, and prevents holistic patient views.
Regulatory Burden
Compliance is essential-but also complex and resource-intensive. Staff often spend a disproportionate amount of time documenting care, completing mandatory reports, and navigating overlapping regulations. Without automation, the risk of non-compliance remains high.
How Operational Shortcomings Impact Patient Care and Costs
Operational inefficiencies are not just administrative headaches-they directly affect the quality of care and the bottom line.
Reduced Quality of Care
Delayed patient intake or discharge processes can lead to overcrowded facilities or rushed care, while communication breakdowns between departments increase the risk of medication errors or missed follow-ups. Additionally, inadequate documentation may compromise the continuity of care across providers, impacting overall patient safety and outcomes.
Staff Burnout
Nurses, physicians, and support staff are burdened with administrative tasks that pull them away from direct patient care. Repetitive work, constant follow-ups, and inefficient tools contribute to rising burnout levels and high turnover rates.
Increased Operational Costs
Every inefficiency-whether in processing claims, managing inventory, or complying with audits-translates to increased costs. Delayed reimbursements, unbilled services, inventory waste, and regulatory penalties are all common financial drains.
Missed Opportunities for Improvement
Without real-time data and integrated systems, healthcare leaders lack visibility into performance metrics. This hinders proactive problem-solving, innovation, and service quality enhancements.
The Need for Operational Transformation
To provide high-quality, value-based care in today’s demanding healthcare environment, organizations must modernize their operations. This means moving away from fragmented, manual processes toward unified, intelligent systems that enable agility, automation, and collaboration.
This is where no-code platforms come in-offering a new, accessible path to transforming operations from the inside out. As we explore in the following sections, no-code technology is not just a workaround for IT backlogs-it's a catalyst for culture change, staff empowerment, and healthcare excellence.
Understanding No-Code Technology
No-code platforms are software development environments that allow users to build applications, automate workflows, and integrate systems through intuitive visual interfaces-such as drag-and-drop builders, pre-configured templates, and rule-based logic-without writing any code. Unlike conventional programming, which requires deep technical expertise, no-code tools are designed for “citizen developers” such as healthcare professionals, administrators, and operational staff who understand domain challenges firsthand.
Key features of no-code platforms include:
- Visual Development Interfaces: Users assemble applications using graphical components like buttons, forms, and workflow diagrams instead of coding languages.
- Pre-Built Templates and Components: Ready-to-use modules accelerate the creation of common healthcare workflows, such as patient intake forms or billing processes.
- Integration Capabilities: No-code platforms often support seamless connections with existing electronic health records (EHR), billing systems, or third-party APIs to enable data flow without manual intervention.
- Rapid Deployment: Applications can be built, tested, and launched in days or weeks, rather than months or years.
- User Empowerment and Collaboration: Clinicians and operational teams can directly contribute to solution design, reducing dependency on IT departments and improving alignment with real-world needs.
- Scalability and Governance: Modern no-code platforms include built-in security, compliance management, and version control, crucial for healthcare's regulatory landscape.
Differences Between No-Code, Low-Code, and Traditional Software Development
While no-code is sometimes grouped with low-code under the umbrella of “visual development,” there are important distinctions:
- No-Code: platforms enable full application creation with zero coding required. They prioritize ease of use and are tailored for users with no programming background. This makes no-code ideal for rapid prototyping, workflow automation, and citizen development in environments with evolving requirements.
- Low-Code: platforms provide a visual development environment but allow (and often require) some hand-coding to customize advanced features or integrations. Low-code is generally geared toward professional developers aiming to accelerate development cycles, offering greater flexibility but still demanding technical expertise.
- Traditional Software Development: involves writing source code manually in programming languages such as Java, C#, or Python. It offers maximum customization and control but is time-consuming, costly, and requires skilled developers. Deployment cycles are longer, making it less adaptive to fast-changing operational needs.
The key tradeoff lies in speed and accessibility versus customization depth. No-code empowers non-technical users to solve specific operational problems quickly, while traditional coding remains necessary for highly complex or bespoke systems.
Why No-Code Fits Healthcare's Dynamic and Regulated Environment
Healthcare is a uniquely challenging industry for digital innovation due to:
- Rapidly Changing Protocols: Clinical guidelines, compliance standards, and patient needs evolve continuously. No-code's agility enables healthcare organizations to adapt workflows and processes swiftly without lengthy development cycles.
- Complex Regulatory Landscape: Compliance with HIPAA, GDPR, FDA regulations, and other mandates demands rigorous data security, audit trails, and governance. Leading no-code platforms embed these compliance features, allowing operational teams to innovate while maintaining regulatory safeguards.
- Diverse User Base: Healthcare operations involve clinicians, administrative staff, IT teams, and external partners. No-code fosters collaboration by allowing different roles to contribute directly to application design, bridging communication gaps.
- Resource Constraints: Labor shortages, budget pressures, and IT backlogs are common in healthcare. No-code reduces reliance on scarce developer resources and accelerates time to value, freeing staff to focus on patient care rather than administrative hurdles.
- Integration Needs: Healthcare systems rarely operate in isolation. No-code platforms provide connectors and APIs that facilitate interoperability with existing EHRs, billing systems, and diagnostic tools, ensuring data consistency and seamless workflows.
By empowering frontline users to create and modify applications without code, no-code technology supports a culture of continuous improvement-critical for delivering efficient, patient-centered care in a complex, fast-paced environment.
Real-World Impact: No-Code in Healthcare Operations
Let's explore how no-code platforms are already transforming everyday healthcare functions:
Modernizing Patient Intake
Traditional check-in involves paper forms, manual data entry, and long wait times. With no-code:
- Patients complete digital intake forms via mobile or kiosks
- Data is automatically routed to the EHR or appropriate system
- Staff are alerted to missing documents or red flags
- Multilingual and accessible interfaces improve equity
Outcome: Reduced wait times, fewer errors, and better first impressions.
Streamlining Staff Coordination
Scheduling shifts, handling time-off requests, or reporting incidents can be chaotic. A no-code workflow:
- Allows employees to submit digital requests
- Notifies supervisors and HR instantly
- Integrates with calendars or workforce management tools
- Logs activity for audit purposes
Outcome: Faster approval and clearer accountability.
Automating Compliance and Documentation
Regulatory requirements demand extensive documentation and tracking. No-code solutions help:
- Build automated audit trails for actions and communications
- Trigger reminders for required training or certifications
- Maintain HIPAA-compliant recordkeeping
- Enable instant reporting and exports for regulators
Outcome: Less time for documentation, more for care.
Platform Spotlight: Yoroflow in Healthcare Automation
In an industry where compliance, coordination, and time-sensitive care are critical, healthcare organizations need agile digital tools that work with them-not against them. Yoroflow is a no-code workflow automation platform designed to empower healthcare providers, administrators, and operations teams to digitize and streamline their internal processes-without writing a single line of code.
Whether you're a hospital administrator managing multi-departmental workflows or a clinic needing faster patient intake and discharge processes, Yoroflow provides the flexibility, scalability, and security needed to build and automate workflows tailored to your unique operational requirements.
Key Features of Yoroflow
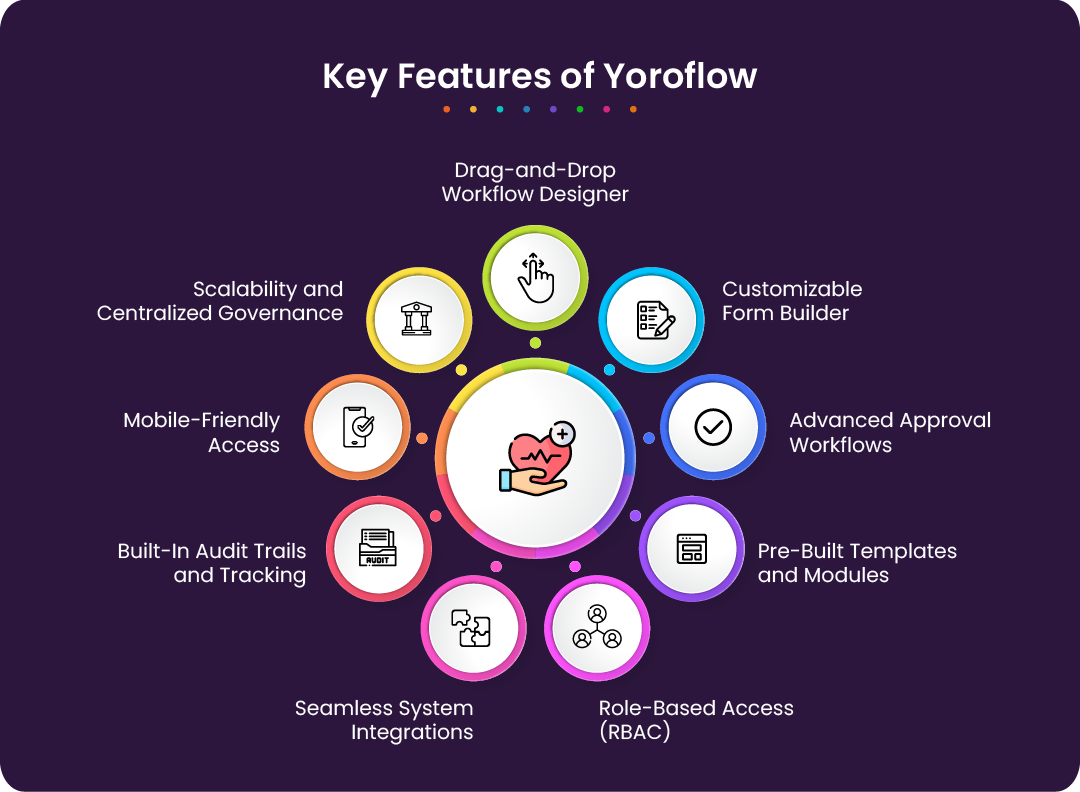
Yoroflow is designed to meet the unique operational and regulatory demands of the healthcare industry. Its no-code framework empowers teams to create, customize, and manage workflows with speed and precision. Below are the key features that make Yoroflow a transformative tool for healthcare organizations:
- Drag-and-Drop Workflow Designer: Easily design and automate complex healthcare processes-from patient admission to discharge, lab testing to insurance verification-using an intuitive visual builder. No coding skills required.
- Customizable Form Builder: Create HIPAA-compliant, responsive digital forms for various use cases such as patient intake, feedback, medication tracking, incident reporting, or staff scheduling. Forms can be embedded into portals or securely shared, ensuring efficient data capture and workflow initiation.
- Advanced Approval Workflows: Set up multi-stage approval processes for equipment requests, policy changes, care plan revisions, or compliance tasks. Define approval chains by roles or departments and automate reminders and escalations to avoid bottlenecks.
- Pre-Built Templates and Modules: Jumpstart automation with ready-made healthcare templates for common workflows like appointment scheduling, inventory management, or compliance documentation. Templates can be easily customized and scaled across teams or facilities.
- Role-Based Access Control (RBAC): Safeguard sensitive information with granular access control. Assign permissions by role or individual user, ensuring that only authorized personnel can view or interact with specific data or workflows-helping you maintain regulatory compliance.
- Seamless System Integrations: Integrate effortlessly with electronic health records (EHRs), customer relationship management (CRM) systems, email tools, and internal databases to streamline data exchange and eliminate duplication.
- Built-In Audit Trails and Tracking: Automatically log every action and workflow update, enabling full traceability. These detailed audit logs support internal reviews, regulatory audits, and ensure accountability across your organization.
- Mobile-Friendly Access: Enable healthcare teams to initiate or manage workflows from any device. Whether on-site, between departments, or in the field, staff can stay connected and productive through mobile interfaces.
- Scalability and Centralized Governance: Designed to grow with your organization, Yoroflow supports enterprise-wide scalability. Centralized governance, data retention policies, and environment management ensure operational consistency and security across all departments and facilities.
With Yoroflow, healthcare organizations can replace manual, fragmented processes with intelligent automation-improving operational efficiency, reducing administrative burden, and enabling staff to focus more on what matters most: delivering quality patient care.
Why Yoroflow?
Yoroflow empowers healthcare organizations to take control of their digital transformation-quickly, securely, and without technical complexity. Unlike traditional software development, which can take months to implement, Yoroflow allows teams to build and deploy powerful workflows and applications in a matter of days. Its intuitive, no-code interface means staff from any department can automate tasks and streamline operations without writing a single line of code.
Security is foundational to Yoroflow's design, with features that align with HIPAA regulations and enterprise-level data protection standards. Built with healthcare in mind, it ensures patient data remains confidential and workflows stay compliant.
Behind the platform is a team with deep expertise in both healthcare operations and automation technology, providing ongoing support and guidance.
Yoroflow transforms healthcare teams into innovators-enabling them to design and manage their own solutions, reduce IT dependency, and accelerate better outcomes for patients and providers alike.
How Yoroflow Enables Rapid Workflow Creation Without Coding
Yoroflow empowers healthcare professionals to build and adapt workflows on their own terms-without relying on developers or navigating complex programming languages. Through its intuitive drag-and-drop interface, users can design workflows for tasks such as patient intake, medical equipment requests, discharge planning, and compliance reporting with minimal effort.
Each step in a workflow can be configured visually, including logic rules, approval paths, automated notifications, and data validations. This makes it easy to implement new processes or adjust existing ones in response to policy changes, staffing updates, or evolving regulatory requirements.
Key Benefits
- Improved Efficiency: Routine and repetitive tasks are automated, reducing manual errors, speeding up service delivery, and allowing staff to focus more on patient-centered care.
- Reduced IT Backlog: Business teams can create and manage their own digital processes, easing the burden on IT departments and accelerating innovation across the organization.
- Enhanced Collaboration: With a shared visual platform, departments can collaborate on designing workflows, ensuring alignment between administrative, clinical, and compliance functions.
By eliminating the traditional barriers to software development, Yoroflow enables healthcare organizations to move with agility-responding quickly to challenges, optimizing operational performance, and continuously improving how work gets done. It transforms process ownership from IT to the people closest to the problems, unlocking faster results and more resilient healthcare systems.
Overcoming the Barriers to Adoption
Every innovation comes with perceived risks. Here’s how healthcare organizations can address common barriers:
Security & Compliance
Yoroflow supports encryption, access control, and audit logging. Ensure your platform is HIPAA-compliant and allows for proper governance.
User Training
No-code is intuitive, but onboarding and change management are crucial. Offer workshops or identify “no-code champions” within departments.
IT Alignment
Position no-code as a collaborative asset, not a replacement. Involve IT in platform selection and integration setup.
Scalability Concerns
Modern no-code platforms are built to scale. Establish governance protocols early and review workflows periodically.
Action Guide: Getting Started with No-Code

Adopting no-code tools can significantly improve operational efficiency in healthcare-but success begins with a strategic, step-by-step approach. Here's a simple five-step plan to help healthcare leaders get started:
Step 1: Identify Friction Points
Begin by mapping out repetitive, manual tasks that burden staff or slow down care delivery. Focus on areas like appointment scheduling, internal approvals, or document handling where inefficiencies are most visible.
Step 2: Engage Stakeholders
Bring together operations, IT, clinical staff, and compliance early in the process. Their input will ensure the solution meets real-world needs and adheres to security and regulatory standards.
Step 3: Choose a Platform Like Yoroflow
Select a no-code solution based on ease of use, integration capabilities, HIPAA readiness, and vendor support. Yoroflow is built with these priorities in mind.
Step 4: Pilot a Use Case
Start with a small project-like digital patient intake or internal supply requests. Measure adoption, user feedback, and time saved.
Step 5: Scale Responsibly
Expand gradually, and implement a governance model to ensure consistency, compliance, and long-term success across departments.
The Time Is Now: Transforming Healthcare Operations with No-Code
The challenges facing healthcare are too urgent to wait for traditional IT timelines. According to a recent Deloitte study, 73% of healthcare executives say their organizations are under pressure to accelerate digital transformation, yet many are held back by limited developer resources and legacy systems.
No-code platforms like Yoroflow offer a powerful, secure, and scalable path to innovation-one that democratizes technology and includes everyone in the organization. By enabling frontline staff to solve operational challenges directly, no-code shifts healthcare from a reactive posture to a proactive, agile model.
The impact is clear: Hospitals that adopt automation report up to 30% improvement in operational efficiency, according to a McKinsey & Company report on healthcare operations. Likewise, organizations leveraging no-code platforms experience deployment speeds up to five times faster than traditional development methods, as highlighted in a Forrester Research study on no-code adoption. The result? Happier teams, improved compliance, lower operational costs-and most importantly, better patient care.
Now is the time to act. Whether you're a small clinic or a large health system, no-code is your invitation to lead the future-not follow it.